Project reports
The Cap Anamur project reports describe the work of our teams on site, provide insights and depict current developments in the aid project.
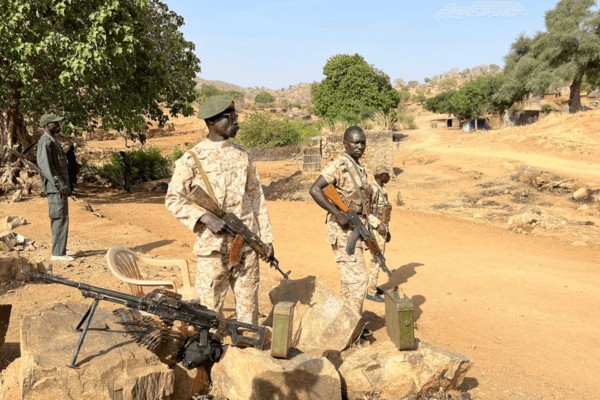
In the shadow of global conflicts and natural disasters, the humanitarian crisis in Sudan is often overlooked by the public. Sudan has been a theatre of armed conflict for decades. However, the renewed fighting that flared up in April 2023 has drastically increased the need for humanitarian aid.
The humanitarian situation in Sudan has been extremely precarious for many years
The political situation in Sudan has been unstable for decades. A 22-year civil war from 1983 to 2005 and 30 years of authoritarian rule divided the country. In 2011, South Sudan seceded from the rest of the country. Since then, there have been repeated armed clashes between rebel groups and the government.
These ongoing conflicts have prevented the country from developing a stable security system and there is no reliable infrastructure. Healthcare in the country is unevenly distributed, which means that a large proportion of the population does not have adequate access to medical care. As a result, life expectancy in Sudan is low and mortality rates among mothers, children and newborns are high.
The healthcare system in Sudan is completely inadequate
There is a lack of health services, particularly in rural areas that have been affected by conflict for many years, including in the Nuba Mountains. In the entire region, which is home to an estimated 2 million people, there are just two hospitals where surgical procedures such as caesarean sections can be performed. One of these is the Cap Anamur hospital. Around 80 % of households live more than an hour away from the nearest health centre. Very few people have cars or other means of transport. Even in the event of serious illness or labour, many people have to walk for hours to the nearest healthcare facility or are carried there on the shoulders of relatives.
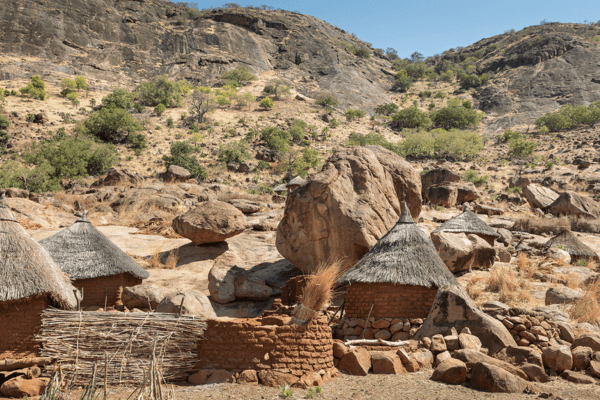
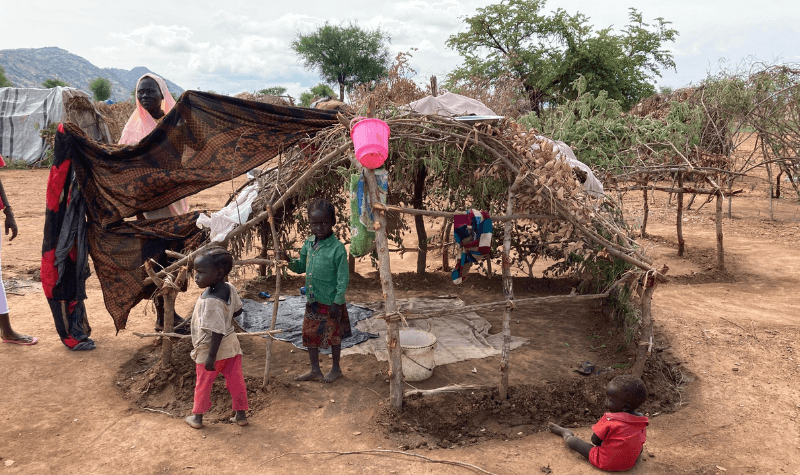
The Nuba Mountains became a refuge for hundreds of thousands of people
Decades of fighting have forced millions of people in Sudan to flee their homes. Around 897,000 internally displaced persons have found refuge in the Nuba Mountains. The resurgent conflict has led to a significant increase in displaced persons since May 2023, exacerbating the challenges in the region and drastically increasing the need for humanitarian aid.

Cap Anamur is still in Sudan to provide humanitarian aid
The fighting in the Nuba Mountains is now palpable and the situation in the region remains extremely unstable and calls for urgent humanitarian support. Our Cap Anamur team is therefore still working in Sudan and supporting the civilian population. In addition to providing medical care for patients in our hospital, we also support people fleeing the war through our mobile clinic. We are constantly expanding the care capacities in our hospital. We recently built a new paediatric ward. The increasing number of malnourished children in particular are optimally cared for there.