Women in Sudan – Cap Anamur Improves Women’s Health
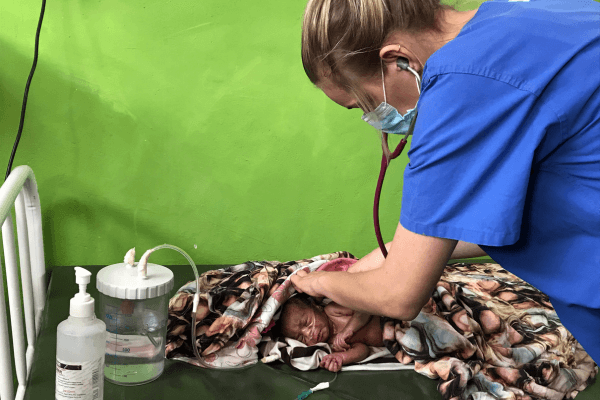
Deployed midwives or gynecologists are regularly on duty at our hospital in Sudan. They assist in the care of pregnant women and provide obstetric care. They also train local midwives, who now provide professional care for many of the births.
Sophie Kellner worked as a midwife in the Nuba Mountains for 8 months. She reports about the work in our hospital in the Nuba Mountains and how important medical help is during pregnancy and births.
Women in Sudan receive intensive care in our hospital during pregnancy and childbirth
Pregnancy and childbirth are a special phase in a woman’s life, which is why professional medical help is essential during this time. Over the past two decades, approximately 10.7 million women worldwide have died from complications during childbirth. More than two-thirds of these deaths occurred in sub-Saharan Africa. Almost all of these deaths could have been prevented by seeking professional obstetric care. Therefore, Cap Anamur offers intensive care to women in Sudan with its own mother and child ward in the hospital in the Nuba Mountains.
Unfortunately, not every woman in the world has the opportunity to give birth to her child in safety and under medical care. The consequences are often catastrophic and not infrequently lead to the death of mother or child. There are many reasons why women do not seek professional obstetric care. Barriers in the Nuba Mountains include lack of transportation, high transportation costs, and long distances to health facilities. The women sometimes have to walk for days or have to be brought to the hospital on a motorcycle or even a donkey in case of obstetric emergencies.

Women in Sudan continue to experience high risk births
Although maternal mortality has declined significantly worldwide in recent years, Sudan is one of the countries in Africa where childbirth continues to be associated with high risk for the mother and the newborn. Sudan has been the site of armed conflict for decades, making the region partially inaccessible, which poses a major risk to health care for the nearly 2 million residents in the Nuba Mountains. There is a lack of basic necessities, such as health care, clean drinking water and education. Women living in the Nuba Mountains in particular suffer from the conflict: they have little or no access to contraceptives, adequate prenatal care or emergency obstetric care. Most women give birth at home (91%) and 30% of them even without any assistance. Especially with regard to the current fighting in Sudan, people’s health is in great danger and the already precarious health situation is massively aggravated. Pregnant women and young children are particularly affected.
Cap Anamur makes a significant contribution to improving women’s health in the Nuba Mountains
I was privileged to experience an educational and formative time as a midwife in the mountains, which had a significant impact on my view of the world.
The fact that access to obstetric care is very difficult for women in the Nuba Mountains became particularly clear to me during a visit to one of our outposts. Never before have I been in such a remote place. We drove for almost 9 hours on roads in disastrous condition, through sandstorms, beautiful palm landscapes and dry, dusty riverbeds, past bombed houses and schools covered with bullet holes – the remnants of war. Sometimes we didn’t meet a single person for hours.
The hospital in Korongo is beautifully located: in a huge valley, surrounded by magnificent mountains. The people from the hospital are insanely nice and hospitable like all Nuba. I share a room with two beds with the midwife and the nurse, there is no electricity, no light, of course no internet, no running water, hardly any medical equipment and only the medicines we brought with us. That night, the midwife called me into the maternity to ask for help because she wasn’t sure about an exam finding. Unfortunately, there was no ultrasound machine to determine the position of the child and to detect the fetal heart sounds there was only a wooden ear trumpet. It was only through our traditional midwifery skills – palpation of the baby through the abdominal wall – that we discovered that they were twins and that the leading baby was in the breech presentation, which posed a major obstetric difficulty. So there I was, facing this obstetric emergency, with no medical equipment, no surgical backup, and the nearest hospital a 9-hour drive away! It was clear to me that if a C-section was necessary to save her life, I would have to watch her die. I would have to watch the woman die.
The birth of the first child took a long time and was complicated. When the little boy was born he needed our support because he could not breathe sufficently. Fortunately, midwife Khaltouma is a great and very experienced midwife and we can work very well together despite language barriers. When the second twin was finally born, we were able to put both children in the arms of the exhausted mother and I could breathe a sigh of relief. I don’t think I’ve ever been so relieved!


