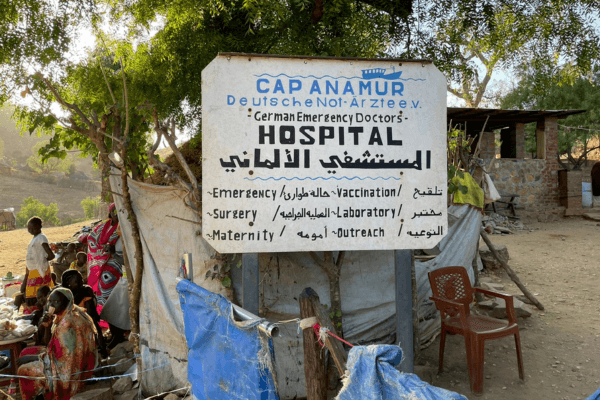
The Right to Health – An interview by Cap Anamur on World Health Day 2024
The motto of this year's WHO World Health Day is "My health, my right". Cap Anamur supports this human right by building and operating health facilities and sending medical personnel. Nevertheless, we need to take a critical look at the global causes and flaws in the system and work on long-term solutions.
On April 7, the WHO calls for World Health Day. The motto for 2024 is “My health, my right”. Cap Anamur / German Emergency Doctors has been pursuing this human right to health since its foundation by creating access to health facilities in various project countries and optimizing the medical treatment of the population through seconded medical professionals. But apart from our successes, we do not want to lose sight of global conditions and systemic problems. We asked our new project coordinator Ole Hengelbrock 10 questions in an interview in which he takes a critical look at the international problems and possible solutions to the human right to health:

1. The theme of World Health Day is “Right to Health”. Is this a new claim?
In principle, everyone has the right to timely and appropriate healthcare. This is an integral part of the right to life and the right to live in dignity. Around 140 countries recognize health as a human right in their constitutions. The WHO’s main objective is to realize “the highest attainable standard of health as a fundamental right of every human being”.
2. What is the current state of implementation, are there any positive developments?
According to a recent United Nations report, the number of children dying before their fifth birthday has reached an all-time low. The mortality rate has fallen by 51 percent worldwide since 2000. Countries such as Cambodia, Malawi, Mongolia and Rwanda are examples of the progress that can be made if appropriate priorities are set and sufficient resources are allocated to medical care. However, this is no reason to celebrate…
3. What does the other side of the coin look like?
A look at the report shows that almost half of the deaths are newborns with preventable or treatable causes, such as pregnancy complications, meningitis, diarrhea malaria or measles.
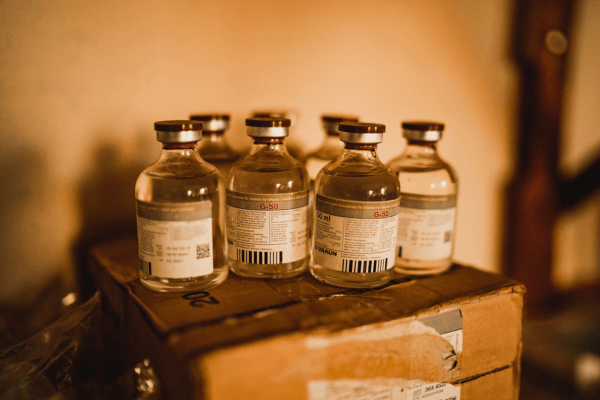
4. Speaking of measles, the lowest vaccination coverage rate for the first measles vaccination since 2008 has been recorded worldwide.
Yes, and since 2016 there have been new outbreaks in ten countries where the spread of measles had been halted. It should be noted that an infection not only implies the disease caused by the virus, but also damages the immune system in general. Up to half of the antibodies present can be destroyed. This means greater susceptibility to germs that cause illnesses such as pneumonia or influenza. But where can the approximately 4.5 billion people – more than half the world’s population – who do not have full access to basic health services go in such cases? In the reality of their lives, accessible health services simply do not exist, are only available in rudimentary form or are rarely affordable in exchange for hard currency. I would like to avoid the word “actually”. But according to the so-called Sphere Standards, at least 80 percent of the population should be able to reach basic medical care within an hour’s walk of their home. Transportation for emergency transfers should be available 24/7. There should be one district hospital per 250,000 inhabitants; now I say: actually!
5 Where is there a particular gap between aspiration and reality?
That is difficult to weigh up against each other. “All tears are salty”, as Janusz Korczak says. But a look at Sudan, Ukraine, Myanmar or Venezuela is disturbing. For nine years, bombs have been destroying the medical infrastructure in Yemen, while at the same time prices for food, water and gasoline have risen by 600 percent. Water pumps cannot be put into operation, resulting in epidemics of diseases such as cholera. In Syria, too, waves of infection occur again and again due to the constant impoverishment of the population, the ailing health system, the destroyed sewage systems and the disastrous hygienic conditions. This is also a consequence of the sanctions policy, which does not target specific groups or individuals, but holds the civilian population hostage across the board. In the Tigray conflict in Ethiopia, people have died as a direct result of violence, but also as a result of hunger and a lack of healthcare.
Wars have disastrous interdependencies: Displacement, overcrowded and inadequate shelter, poor sanitation, insufficient water quantity and quality, and reduced food security are all factors that increase the risk of malnutrition and outbreaks of communicable diseases. In addition, extreme stress factors, such as experiences of loss and violence, endanger mental health. An interrupted supply of medication stops ongoing treatments for HIV, tuberculosis, diabetes and mental illness. If you want to better fulfill the right to health on a large scale, you have to work on conflicts and how to end them.
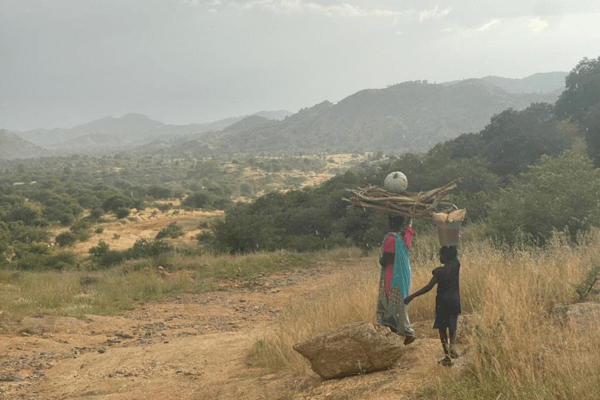
6. What is the situation in countries that are not at war?
Late treatment is a widespread problem with often fatal consequences. Many patients only arrive at the hospital after a long odyssey in a highly critical condition. Either it is the difficult transportation route, for example when rainy seasons wash out the roads, or volatile violent actors that make routes impassable. Another reason for the late arrival are the feared costs. In addition to the transport, the stay in hospital for several days, the loss of labor at the market or in the field, the treatments, medication and blood reserves have to be covered. This is not covered by insurance and only in rare cases do people have their own financial reserves. In Sierra Leone, blood transfusions are only possible if a relative donates blood as a reserve. One bag for one bag. The scene is repeated daily, in which relatives who have already donated negotiate with people outside the clinic to allow further transfusions in exchange for cash. Health is a value. If this is linked to debt, it does not just mean financial losses for people in many regions of the world, but existential threats. The fear of debt sometimes makes people hesitate for as long as possible. And sometimes they simply don’t have the means to even consider a trip to hospital or a second blood transfusion.
7 Who is responsible for changing this?
For me, the reference to the principle of subsidiarity, according to which the state is primarily responsible for the protection and care of the population, fails because of the established power structures on the ground, which sometimes enrich themselves with the country’s wealth of resources without expanding the social security system and medical infrastructure. If you think “It’s their own fault, then they can help themselves”, I would like to counter that: Firstly, it is becoming more difficult for populations in many regions of the world to stand up for their rights. Only two percent of the world’s population live in states with unrestricted civil liberties, while more than two thirds live in authoritarian states or dictatorships. The scope for legal claims is limited. Secondly, pointing the finger at those in power at the local level inevitably goes hand in hand with the theft of raw materials and overreaching through trade agreements with Western countries.
8. Please elaborate, an example?
The post-colonial discourse needs to be included when we talk about responsibility. While 56 French nuclear power plants export nuclear power and generate taxes for the common good, 81.4 percent of the population of Niger is excluded from the electricity grid, according to the World Bank. Around a third of French and a quarter of European uranium imports come from Niger, the seventh largest uranium producer in the world. These are exploitation dynamics that are concealed by state aid and whose consequences are only mitigated to a small extent, if at all. Much would be gained if unfair clauses in economic agreements and non-transparent trade relations were made fairer. The problem of “brain drain” is also critical, the poaching of skilled workers from countries in the global South, with which industrialized countries try to close their own supply gaps. In recent years, the recruitment of international staff in the healthcare sector has increased significantly. There will be a shortage of up to 150,000 nurses in Germany by 2025. Industrialized countries like to describe themselves as “donors” because of their international aid payments, but first and foremost we are “recipients”.
9. What about “giving” in order to realize the main goal of “the highest attainable standard of health as a fundamental right of every human being”?
The stumbling block called dependency lies in the financing of the WHO. There are compulsory state contributions that are calculated according to the gross national product and the economic situation of the respective country – Germany paid 58 million US dollars in 2022 and 2023. However, the WHO budget is largely funded by voluntary contributions, sometimes five times as high as the compulsory contributions and mostly earmarked for specific purposes. These funds are earmarked for a specific topic or a selected region. Last year, less than a fifth of the funds were spent autonomously. The financiers play a decisive role in defining what is highly achievable and which health standards are a fundamental right, when, where and how. Incidentally, Germany’s contributions are falling again. Other member states are also reducing, paying compulsory levies irregularly or not at all, which leads to unpredictability and cutbacks. The affairs of the WHO can only be dealt with to a limited extent due to the institutional funding crisis.
10. For an outlook, what should and can be done for the right to health?
Well, spending targets are currently popular. The EU spending target of 0.25 percent of GDP for Ukraine is described as “sympathetic”. NATO’s two percent target, originally a freely set target, has been set in stone and is backed by special funds. States are to spend 0.7 percent on development cooperation and humanitarian aid. Germany only meets this target due to a highly questionable calculation basis, which includes internal accommodation costs for refugees or the cost of university places for people from the Global South. This calculation trick has made Germany the largest recipient country of its own aid, with around 6.3 billion US dollars remaining in the Federal Republic. Perhaps someone will finally come up with a fixed spending target for compulsory contributions. Then at least more independent decisions could be made. Another step is to work harder on conflicts and their resolution. This in no way legitimizes spirals of armament, as the current jargon suggests, as more militarization is demonstrably at the expense of other issues such as health and social issues, as a comparison with the “Global Health Security Index” shows. Trade agreements must also be negotiated more fairly in future; the word “right” is in there.
Whatever happens or fails to happen, there will always be niches and situations of state collapse in which civil society actors such as Cap Anamur must be concretely and actively involved in order to realize healthcare that is available, accessible, acceptable, affordable and of good quality. Unfortunately, this task will not stop! However, this work is by no means “normal”. The need to work in wars and crisis contexts, i.e. to provide humanitarian aid, is not a substitute for politics and legal regimes, but a sign of their failure. If this is compounded by an inability or even unwillingness to help as needed (including dropping aid from airplanes), this is ultimately an expression of the collapse of rights. From this low point, the people affected are looking at the basic right to health. We should not lose our ability to be offended by these circumstances!

